What is Von Hippel-Lindau disease?
Von Hippel-Lindau disease (VHL disease) is a rare genetic disorder in which multiple tumors and cysts can grow in various parts of the body.
11.04.2024
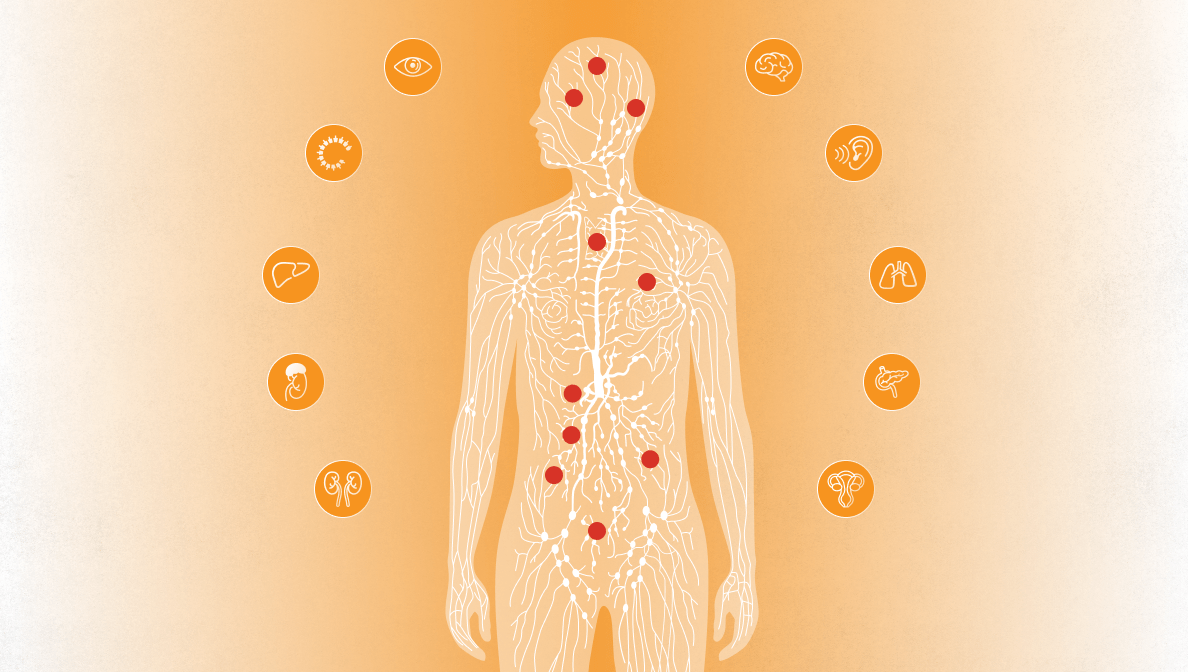
Von Hippel-Lindau disease (VHL) is caused by a genetic defect that leads to the development of various, mostly benign tumors (accumulations of tissue) and cysts (fluid-filled cavities in tissue). They can often occur in the brain and spinal cord, in the retina, in the kidneys, in the pancreas, in the inner ear, but also in other parts of the body.
If left untreated, the disease can be life-threatening.
VHL disease is rare
VHL disease occurs in about one out of 36,000 people. Around 200,000 cases are known worldwide. The precise time at which the first signs of the disease appear and how severe the course of the disease is can vary greatly.
At the time of diagnosis, those affected are on average 26 years old. In around 97% of people with a VHL gene mutation, symptoms appear by the age of 65. Men and women are equally affected.
Cause of the disease
The cause of Von Hippel-Lindau disease is a defect in the so-called VHL gene.
In healthy people, the VHL gene produces a protein that prevents the development of tumors. In people with Von Hippel-Lindau disease, this gene does not function as it should. It cannot produce enough protein to prevent tumor formation.
In most cases, VHL disease is inherited
Von Hippel-Lindau disease is inherited in a manner known as “autosomal dominant”.
- This means that if one parent has a defect in the VHL gene, each of his/her children has a 50% chance of inheriting this gene and developing the disease.
- Approximately 80% of affected people have a parent with VHL disease.
- In around 20% of those affected, VHL disease occurs without either parent being affected.
Clinical presentation
VHL disease is also known as “multisystem disease”. This is because several tumors and cysts typically grow in various organs.
Most VHL tumors are benign. However, as they grow larger, they can cause discomfort and pain and, if left untreated, they can significantly impair quality of life.
Possible medical findings in VHL disease:
- Tumors in the brain and spinal cord
They can cause headaches, dizziness, and neurological symptoms. - Tumors in the retina
They can lead to visual impairment. - Kidney diseases
These include kidney cysts and renal cell carcinomas (kidney cancers). - Pancreatic diseases
They include cysts and tumors in the pancreas. - Tumors and cysts in other organs, such as the liver, lungs, or reproductive organs.
Important: the clinical presentation varies from person to person. The age of onset and the course of the disease also vary from person to person.
Diagnosis
There are indications and criteria that may indicate VHL.
These include:
- Family history
There are cases of VHL or other genetic tumor diseases in the family.
- Ongoing tumor diseases
Presence of cysts and tumors in various organs in the body..
Since the disease is caused by a genetic defect, genetic testing is crucial to confirm the diagnosis. Individuals with a genetic predisposition to VHL should be closely and regularly monitored by a team of specialists from various disciplines.
Therapy
Thanks to intensive research in recent years, medical knowledge and therapy options for treating VHL disease have significantly improved. Nevertheless, the treatment remains complex. The main aim is to remove tumors and cysts, if possible, to reduce their size or stop their growth before they become so large that they cause permanent discomfort.
Treatment options include:
- Surgery to surgically remove tumors or cysts.
- Laser therapy for certain tumors, for example of the eye.
- Radiotherapy to reduce the size of the tumor.
- Radiofrequency ablation (RFA), a procedure in which cancer cells are killed by heat.
- Medication therapies to contain tumor growth.
The suitability and timing of these treatment options vary from person to person and depend on the specific tumors, symptoms, and overall health condition.

Information for medical professionals
For further information on MSD medicines and vaccines, please visit mymsd.ch, the web portal exclusively for medical professionals.

Information for patients
Are you looking for information about specific diseases, their causes, symptoms, prevention or treatment? Discover msd-gesundheit.ch, the information platform exclusively for patients.
CH-NON-02547, 02/2024